Microneedles are nothing new in drug delivery. Since the 1990s, research groups have been studying their potential as an alternative to pills or injections. Their promise is clear: while oral drug delivery can lead to problems with bioavailability, and injections can be painful, microneedles are painless and minimally invasive. A wide range of different drugs, including vaccines, could in theory be self-administered through the skin.
Just as the name suggests, microneedles are tiny needles, grouped together in large numbers (an array). The drug is placed in, or on, the microneedle tip, and the patch is applied to the outermost layer of the skin without reaching the pain receptors.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
There are many advantages, not least the ease of administration and good tolerability. What’s more, the intradermal space is rich in immune cells, which could lead to an improved antibody response in the case of vaccines.
“Humans have 100 to 1,000 times more migratory immune cells in that epidermis space we do in the muscle, and those are the target cells for vaccines,” says Joseph DeSimone, professor of translational medicine and chemical engineering at Stanford University. “Getting your cargo to where you need it is really an advantage.”
Especially since the start of the Covid-19 pandemic, microneedles have come to the fore as a promising mode of vaccine delivery. They could be used to immunise large populations without the need for hypodermic needles, potentially increasing vaccine uptake.
Problems with microneedle manufacturing
Unfortunately, microneedles have so far failed to live up to their potential, with the majority of commercial applications confined to skincare and cosmetics. Time and again, researchers have faced technical challenges at the manufacturing stage, while others have struggled with delivering a reliable dosage.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData“A microneedle array is nothing like a syringe needle,” says DeSimone. “The syringe is inserted, and every drop of liquid is 100% delivered into the muscle. That doesn’t happen reliably with typical microneedle arrays.”
As he explains, there have been three phases in microneedle manufacturing technology. First generation microneedles were fabricated in the 1970s using the tools of the microelectronics industry.
“It fell short in scaling because it’s expensive, and the materials used in the microelectronics industry limited the geometries that one could make,” says DeSimone.
After that came the second generation of microneedles, which was driven by moulding technologies and led to early applications within drug delivery. You start by creating a silicone template, and then take a mould that looks akin to an ice cube tray. This in turn is used to mould replicas of the original silicone shape.
While this technique gave rise to a wide range of chemistries, including dissolvable microneedles, it too failed to scale and reach its commercial potential.
According to DeSimone, the moulded microneedles weren’t as sharp and crisp as their microfabricated predecessors. They lacked mechanical robustness, and fractured easily. On top of that, they suffered a ‘bed of nails’ effect, meaning it took a lot of insertion force to press the patch into the skin. Taken together, these factors exacerbated the dosage problem.
It is only recently that third-generation technologies have started to emerge. For players in this space, the race is on to find new approaches and designs, which could finally bring microneedle-based drug delivery into the mainstream.
“Our raison d’etre is using direct fabrication technologies to convert microneedle microarray patches to a reliable and reproducible dosage form,” says DeSimone.
He adds that 3D printing technologies were formerly limited to prototyping, because they are slow and had poor resolution. His team has figured out how to print much more quickly, and at far higher resolutions.
How 3D printing could help
In September 2021, DeSimone’s lab at Stanford reported on their new 3D-printed microneedle vaccine patch. They used a 3D-printing technique called continuous liquid interface production (CLIP) to create microneedles with complex geometries.
Whereas moulded microneedles look like cones, these are lattice structures, somewhat like the Eiffel Tower. This increases their surface area, and paves the way for new dry vaccine formulations (in this case, a sugar solution). That in turn could simplify storage and eliminate the need for cold chain.
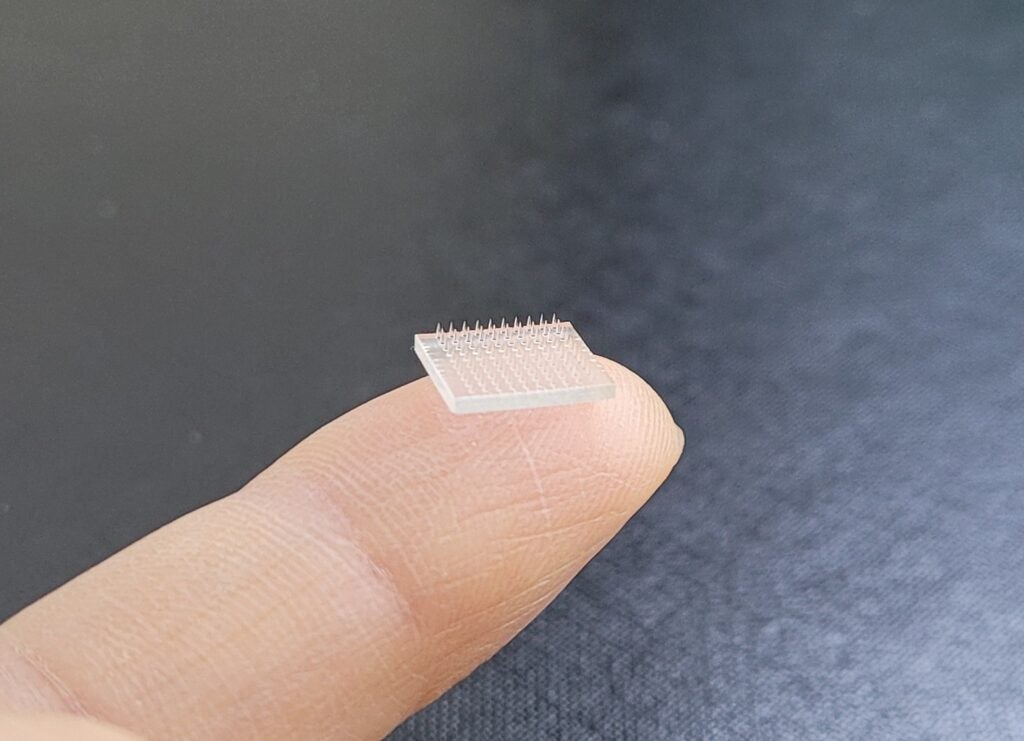
“The cargo is entrapped in these lattices in ways that you couldn’t do before,” says DeSimone. “You can make the needles five different heights and lower the insertion forces by a factor of five, eliminating the bed-of-nails problem. They’re very safe to use, because you can make them out of advanced materials that don’t fracture.”
The researchers tested their patch on mice, and found that it achieved a very strong immune response – 50 times stronger than the same amount of vaccine delivered subcutaneously. If the same holds true in people, that could dramatically reduce the dose of vaccine required.
While their initial research involved a protein-based vaccine, the researchers are now testing mRNA and self-amplifying RNA vaccines. They are being supported in their efforts by the Wellcome Leap Foundation and the Coalition for Epidemic Preparedness Innovations (CEPI).
Devices in development
DeSimone’s lab is far from the only one breaking ground in microneedle-based drug delivery. Currently, GlobalData’s Medical Intelligence Center lists 18 devices of this nature in clinical development or approvals, seven of which are targeted at infectious diseases. GlobalData is the parent company of Medical Device Network.
To cite just a few examples, researchers at the University of Tokyo are developing a Coronavirus Detection Patch, using biodegradable materials, which can detect Covid-19 antibodies in the skin. This would eliminate the need for swab tests.
South Korean startup Jubilee Biotech is applying for patents for its JUBIwatch, a medication management platform that administers specified amounts of medication at set times. The microneedle cartridge is placed inside a smartwatch, which connects to the patient’s medication schedule via a mobile app.
San Diego-based biotech Diomics has reached the approvals stage for its Diocheck Antibody Indicator, which resembles a nicotine patch. The technology can identify whether or not the user has developed Covid-19 antibodies – a useful way of monitoring their level of protection against the virus.
Other devices at the approvals stage include Actuated Medical’s GentleDispense System, which is designed to deliver large molecule compounds (e.g. HIV drugs) into the skin, and Microdermics’ Microneedle Drug Delivery System. The latter is integrated with syringes, auto-injectors and smartpens.
On top of that, several leading institutions are working to develop microneedles for vaccine delivery.
“Over 58 studies are currently registered in the clinical trials database at phase I-IV,” says Dr Ayhan Celik, chief scientific officer at Imperial Bioscience Limited and author of a recent review paper on the subject. “But to translate this innovative technology into feasible products in the relevant markets, some crucial questions should be considered.”
Some of the challenges, he says, are microneedle characteristics, biocompatibility, loading capacity, cost of manufacture and regulatory issues. He believes the latter two factors are the ones most likely to hold the industry back.
“The most advanced drug delivery system using microneedles was rejected by the FDA recently, due to some technical and bioequivalent matters,” he says. “Once a successful example is approved, I think huge number of microneedle-related products will become available soon afterwards.”
Covid-19 vaccines
Within the Covid-19 vaccine space, there are several other microneedle-based devices at the preclinical stage. Early in the pandemic, researchers at the University of Pittsburgh announced they were developing a dissolving microarray patch coated in viral protein. That same month, Verndari and the University of California, Davis, announced they were working on a coated metal vaccine patch.
Later that year, researchers at University of Connecticut followed suit with a transdermal core-shell microneedle system, manufactured in a manner similar to 3D printing. Notably, the needles dissolve at different times, allowing the vaccine to be delivered over a period of days or weeks.
Also worthy of mention is a high-density microarray patch designed by the University of Queensland. In mouse studies, this patch proved highly effective against Covid-19 variants – in fact, it was 11 times better at neutralising the Omicron variant than the same vaccine delivered via needle.
None of these devices have reached the point of commercialisation. However, new manufacturing techniques – along with the added push provided by the pandemic – are creating a renewed buzz within a field that long seemed stagnant.
“The idea that you could receive your Covid-19 vaccine in the mail, as a dry patch you could self-administer – that it was stable thermally, that you could have global access more readily – that’s the vision we’re trying to propagate,” says DeSimone.





