Researchers at Cincinnati Children’s Hospital Medical Center, US and Yokohama City University (YCU), Japan, have developed a process to tissue-engineer human pancreatic islets to treat diabetes in mice and could one day use the technique for human organ regenerative therapy.
Known as self-condensation cell culture, the new process allowed the scientists to create human pancreatic islets that develop a circulatory system, secrete hormones like insulin and can successfully treat sudden-onset type 1 diabetes when transplanted into mice.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
Cincinnati Children’s Center for Stem Cell and Organoid Medicine physician-scientist Takanori Takebe said: “This method may serve as a principal curative strategy for treating type 1 diabetes, of which there are 79,000 new diagnoses per year. This is a life-threatening disease that never goes away, so developing effective and possibly permanent therapeutic approaches would help millions of children and adults around the world.”
Takebe, who along with YCI Colleague Hideki Taniguchi is the study’s co-lead investigator, stressed that their tissue-engineering process will need additional research before it can be used therapeutically in a clinical setting.
The processing system was tested on donated human organ cells, mouse organ cells and induced pluripotent stem cells (iPS) which can act like embryonic cells and form any tissue type in the body.
The process also uses mesenchymal stem cells (MSNs) and human umbilical vascular endothelial cells (HUVECs).

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataThe cells were combined with other genetic and biochemical material that can cue the formation of pancreatic islets and placed in conditions that nourish and nurture cells. The ingredients then condensed and self-organised into pancreatic islets ready to be transplanted into humanised mouse models of severe type 1 diabetes. The transplanted cells were shown to successfully treat the condition.
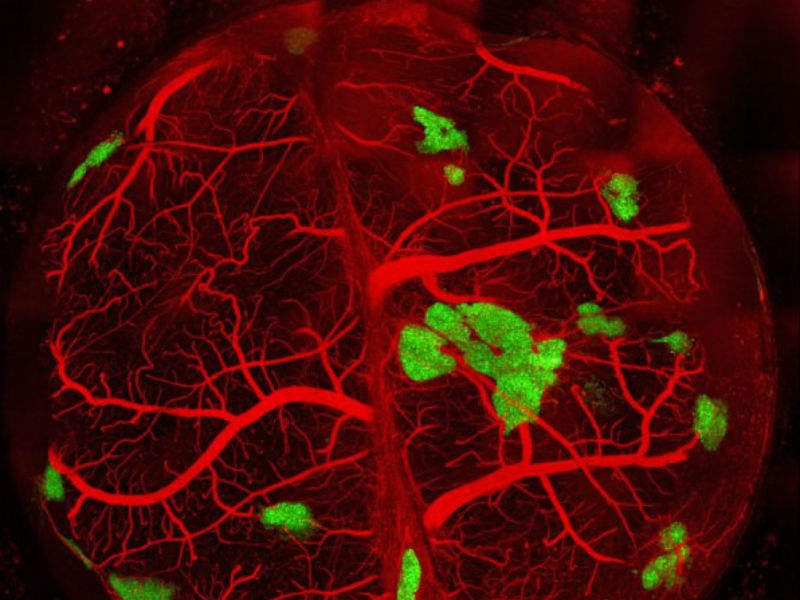
One challenge of successfully applying this process to treat diabetes in humans is that engraftment success rates are relatively low in humans due to the tissues losing their vascularisation and blood supply as they are processed before transplant. This makes it difficult for patients to receive the maximum benefit of these procedures.
Another challenge is ensuring a blood supply to nourish the transplanted tissues.
Taniguchi said: “We need a strategy that ensures successful engraftment through the timely development of vascular networks. We demonstrate in this study that the self-condensation cell culturing system promotes tissue vascularisation.”





